This blog article is about photodynamic therapy with lasers and its benefits and applications.
This article is brought to you by LECC TECHNOLOGY, a global leader in the manufacture of laser solutions for photodynamic therapy and beyond.

Photodynamic Therapy with Lasers: Principles, Benefits, and Key Applications
Photodynamic therapy (PDT) has become one of the most promising minimally invasive treatment techniques in medicine. By combining a photosensitizer with a targeted light source, PDT can destroy harmful cells, deactivate microbes, and stimulate tissue regeneration — all while minimizing damage to surrounding healthy tissue.
When performed with lasers, PDT gains additional precision and consistency, making it suitable for a wide range of medical and cosmetic applications. This article explores the principles of photodynamic therapy with lasers, its clinical benefits, and its most exciting applications across multiple fields of medicine.
How Photodynamic Therapy with Lasers Works
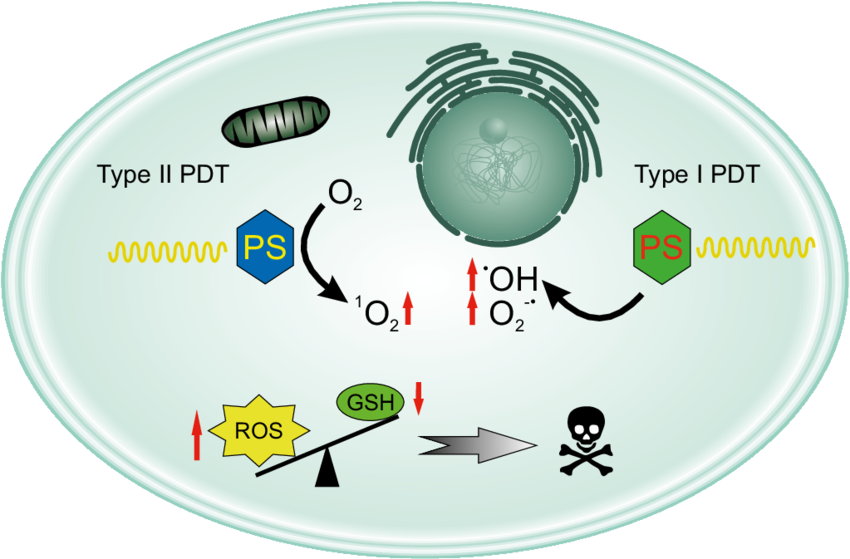
At its core, PDT is a three-component system:
Photosensitizer: A light-activated drug or compound that accumulates in the target area.
Laser Light Source: A monochromatic beam tuned to the absorption peak of the photosensitizer.
Oxygen: Present in tissue and essential for the generation of reactive oxygen species (ROS).
When the laser light excites the photosensitizer, ROS are generated, leading to cell death (in diseased tissue), microbial inactivation, or tissue modulation.
Why Lasers Are Preferred in PDT
Lasers offer:
Precise Wavelength Control – ensures maximum activation of the photosensitizer.
Adjustable Power and Dose – minimizes tissue overheating and allows fine-tuned energy delivery.
Localized Illumination – treats only the intended area, sparing healthy surrounding tissue.
The principles of photodynamic therapy (courtesy of Wolny D., Stojko M., Zajdel A.)
Clinical Benefits of Laser-Based Photodynamic Therapy
One of the most compelling advantages of laser-based photodynamic therapy is its ability to selectively target diseased tissue while sparing the surrounding healthy cells. This high level of precision allows clinicians to treat localized conditions with minimal collateral damage. Because PDT is non-invasive, most procedures can be performed on an outpatient basis without the need for anesthesia or surgery, which greatly reduces recovery time and patient discomfort.
Another important benefit is its remarkably low systemic toxicity. Unlike chemotherapy or long-term antibiotic regimens, PDT’s effects are localized to the illuminated area, avoiding widespread side effects. Moreover, photodynamic therapy remains effective against drug-resistant bacteria and biofilms, offering a promising solution in an era of rising antibiotic resistance. Finally, PDT can be safely repeated multiple times if necessary, making it an excellent option for chronic conditions that require ongoing management.
Key Applications of Photodynamic Therapy with Lasers
Below are the most prominent non-oncology applications where laser-based PDT is showing clinical value.
PDT in Dermatology and Aesthetic Medicine
In dermatology, laser-based photodynamic therapy has proven to be a highly effective approach for a variety of skin conditions. One of its most common uses is in the treatment of moderate-to-severe acne. By targeting Cutibacterium acnes (formerly Propionibacterium acnes) and reducing the activity of sebaceous glands, PDT helps clear breakouts while addressing the underlying causes of inflammation.
Beyond acne, PDT has shown promise in managing chronic inflammatory conditions such as psoriasis. By modulating local immune responses, it can significantly reduce the appearance of psoriatic plaques and bring relief to patients with other persistent dermatoses.
PDT is also making its way into aesthetic medicine. When combined with fractional laser systems, it is used to rejuvenate the skin, diminish fine lines and sun damage, and improve overall tone and texture — offering a non-invasive path to healthier, more youthful-looking skin.
PDT in Dentistry and Oral Health
Laser-based photodynamic therapy is rapidly gaining popularity in modern dentistry as a minimally invasive way to combat oral infections. In periodontal therapy, photosensitizers such as methylene blue are activated with diode lasers to destroy pathogenic bacteria and disrupt biofilms deep within periodontal pockets, leading to improved gum health and reduced inflammation.
The same approach is now being applied to endodontics, where PDT is used to disinfect root canals more thoroughly than conventional irrigation methods, reaching areas that mechanical tools cannot access. Additionally, PDT offers a valuable solution for managing peri-implantitis. By targeting bacteria around dental implants without the need for invasive surgical procedures, PDT helps preserve implant stability and promotes better long-term outcomes for patients.
Antimicrobial PDT (aPDT) for Infection Control
Photodynamic therapy offers a powerful weapon against antibiotic-resistant bacteria by generating oxidative stress that destroys pathogens without relying on conventional drugs. This mechanism bypasses bacterial resistance pathways, making PDT a promising option for addressing multidrug-resistant infections.
In wound care, PDT has shown excellent results in managing chronic ulcers, pressure sores, and diabetic foot wounds. By reducing microbial load and stimulating local tissue repair, it accelerates healing and lowers the risk of infection.
Researchers are also exploring PDT for hospital decontamination. Early-stage systems aim to use light-activated photosensitizers to sterilize medical equipment and even hospital surfaces, potentially lowering the risk of healthcare-associated infections in clinical settings.
PDT in Ophthalmology
Laser-based PDT remains a valuable treatment for wet age-related macular degeneration (AMD) and central serous chorioretinopathy, where it selectively occludes abnormal choroidal blood vessels.
Photodynamic Therapy for Hair Growth
A promising area of research is the use of PDT for hair regrowth. In this application, a photosensitizer is applied to the scalp and activated with low-level laser light.
Mechanism: ROS generation appears to trigger follicular stem cell activation and boost microcirculation.
Early Results: Studies indicate increased hair density and thickness compared to LLLT alone.
Clinical Potential: PDT could become a valuable non-invasive option for androgenetic alopecia and other hair loss conditions.

Laser solution for hair regrowth (courtesy of LECC Technology)
Veterinary Applications of PDT
Laser PDT is increasingly used in veterinary practices to treat infected wounds, oral infections, and even certain skin tumors in pets, with rapid recovery times and minimal discomfort.
Key Parameters for Successful Laser PDT
Photosensitizer Choice: Should match the target tissue and desired depth of penetration.
Laser Wavelength: Must correspond to the absorption spectrum of the drug (often 630–700 nm).
Light Dose (Fluence): Needs careful calculation to maximize effect and minimize tissue damage.
Oxygen Supply: Treatments may be less effective in hypoxic tissues, so oxygenation is important.
Challenges and Future Outlook
While laser-based photodynamic therapy holds significant promise, several challenges continue to limit its widespread adoption. One of the primary hurdles is the limited penetration depth of light in biological tissues. Researchers are actively exploring solutions such as near-infrared lasers and two-photon excitation techniques to extend treatment reach to deeper targets.
Another barrier is the lack of standardized clinical protocols. Variability in photosensitizer dosing, light delivery methods, and treatment timing makes it difficult to compare outcomes across studies, which slows regulatory approval and clinical acceptance.
Cost remains an additional consideration, as both the specialized equipment and photosensitizers can be expensive. However, innovation is rapidly addressing these limitations. Nanoparticle-based photosensitizers promise greater efficiency, wearable PDT devices could enable at-home treatments, and AI-driven dosimetry systems may allow more precise and individualized therapy planning. Together, these advancements are expected to make PDT more accessible, effective, and scalable in the near future.
Conclusion
Photodynamic therapy with lasers is no longer confined to cancer care. It is a versatile and rapidly evolving therapeutic approach reshaping dermatology, dentistry, infectious disease control, ophthalmology, and even regenerative applications like hair growth.
With continued research and standardization, PDT is poised to become a mainstream, patient-friendly treatment modality that bridges light science and medicine.
Selected Literature & References
Hamblin MR, Hasan T. Photodynamic therapy: a new antimicrobial approach to infectious disease? Photochem Photobiol Sci. 2004.
Wainwright M, Maisch T, et al. Photodynamic therapy for infection control: State of the art. J Photochem Photobiol B. 2017.
Calzavara-Pinton P, et al. Photodynamic therapy with topical photosensitizers in dermatology. J Eur Acad Dermatol Venereol. 2012.
Sigusch B, et al. Photodynamic therapy in periodontics: a review. Photodiagnosis Photodyn Ther. 2010.
Avci P, et al. Low-level laser (light) therapy for treatment of hair loss. Lasers Surg Med. 2014.
